Antidepressants and The Biopsychosocial Approach
How many of us have been prescribed a medication without fully being aware of or understanding the impact it has upon our bodies?
By Jessica Young, Featured Writer.
We live in a world of rising mental health struggles with ¼ of people now being diagnosed with a condition each year (MIND, 2017). Depression is sometimes referred to as the common cold of mental ill-health as it is the most prevalent mental illness worldwide, impacting over 3.3./100 people in the UK during 2016 (MIND, 2017).
With the first port of call often being our GPs, limited health resources are becoming further and further strained as the number of individuals struggling mentally continues to rise. However, these growing statistics may reflect a greater willingness from professionals to diagnose as oppose to an increased number of cases. The soaring rates of those requiring mental health support has placed significant pressure on the already limited resources of the NHS, along with the challenges it has to balance with expanding infrastructure. This consequently has negatively impacted the quality of treatment and attention patients receive, resulting in brief medical consultations and somewhat rushed treatment approaches due to cost-effective prioritisation. This combination of events has consequently meant that psychopharmacological treatment methods have dominated the mental health industry as a quick fix in response to these increasing rates.
Many of us who take psychotherapeutic medications to help manage symptoms of mental distress, unfortunately do not possess the knowledge and training to understand exactly what we are exposing our bodies and minds to when we take the pills we are prescribed. Therefore, this article hopes to address the following questions that sit at the forefronts of our minds when it comes to antidepressants:
o Why are we given the medication?
o What are the medications? What do they do?
o How do medications fit within the bigger picture?
Beginning With The Biological Basics:
Within psychology there are five predominant disciplines, one of which is biological; attributing human feelings, thoughts, and behaviours to internal, physiological processes or innate evolutionary characteristics.
As biological organisms we are essentially an overall sum of many small biological components, each contributing to a wider biological framework of systems. There are many biological systems and indicators that have been linked to mental health struggles such as depression. These include heart conditions, brain dysfunction or damage, diseases including Cushing’s and many more. However, for this article we shall zoom in upon some of the chemical imbalances within the brain; one of the key elements underpinning the biomedical approach to interventions and treatments.
Every organ is made up of cells (the smallest structural unit of an organism).
The human brain is a crucial organ consisting of billions of cells with a variety of types, one of the most crucial being neurons.
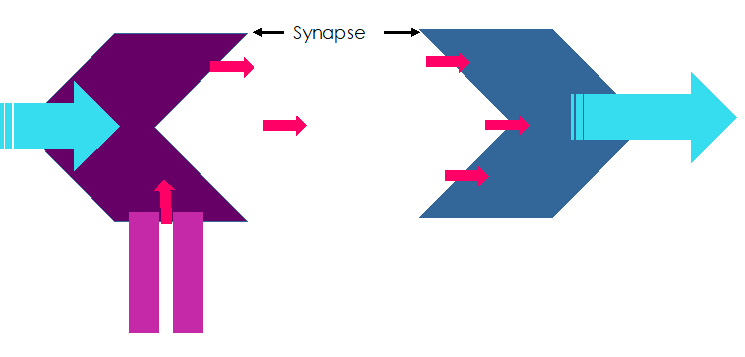
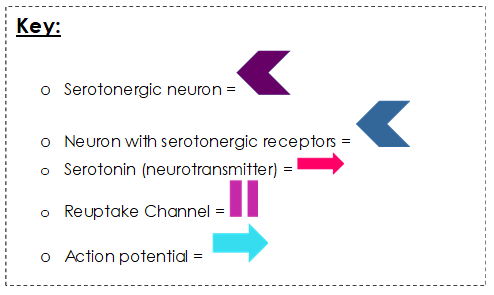
At the point where two neurons meet, there is a small gap known as a synapse. Information must cross the synapse to reach the receptive neurons.
When neuron one receives information in the form an action potential, it releases a chemical known as a neurotransmitter. The neurotransmitters cross the synapse to occupy the receptors at the second neuron. Receptors are attachment points on a neuron, specific to different neurotransmitters.
Once the neurotransmitter is occupying the receptors of neuron two, this triggers an action potential to be released. The process continues throughout the network of intertwined neurons. Each fired action potential continues the passing of information via neurotransmitters.
And how is this relevant to struggling mentally?
There are many related neurotransmitters. A crucial one to focus on is serotonin.
Serotonin is a neurotransmitter which assists in passing information between neurons within the brain, it is released by serotonergic neurons and binds to serotonergic receptors on other neurons. Once released serotonin will travel across the synapse to join receptors upon the receiving neuron. This then triggers the passing on of information from the receptive neuron via action potentials to another awaiting neuron. Excess serotonin not received by the impacted neuron can be re-absorbed via reuptake channels by the original serotonergic neuron; helping to re-stabilise levels. The cycle repeats throughout interconnected systems of billions of neurons.
Low levels of serotonin result in lower activity of associated neurons with less action potentials being fired; levels can be low for many reasons such as an innate under-production. On a larger scale, this means under-activity of the systems consisting of these neurons result in changes to brain activity. This is associated with an increased experience of depression and symptoms such as low mood, disturbed sleep, altered eating habits and so on.
Neuron Function:
There are many biological processes and systems that can be related to mental health struggles, neurotransmitter imbalances are just one; however, chemicals such as serotonin are the target for many medications often prescribed to us.
Offering Some Explanation of Medication:
How many of us have been prescribed a medication without fully being aware of or understanding the impact it has upon our bodies?
Antidepressant Medications (ADMs) are a persistently followed treatment path for depression and other conditions such as anxiety. A neurotransmitter imbalance, such as low levels of serotonin, requires some assistance to obtain healthier function.
Biological aetiology >>> biological treatment, right?
Since their accidental discovery in the 1950s, antidepressant medications (ADMs) have become a dominant treatment option. Monoamines refer to neurochemicals such as serotonin, dopamine and noradrenalin – all of which play crucial roles in many biological processes and have an impact upon experiences of low mood and other symptoms of depression (as well as other mental health struggles). As there are various neurochemicals, neurons, organs, biological systems and so on relating to depression - there are a variety of different ADMs that have been utilised as interventions.
For example:
Tricyclic Antidepressants:
Discovered in the 1950s, tricyclics earn their name by impacting three neurotransmitters: norepinephrine, serotonin, and acetylcholine. By increasing levels of the first two, and blocking the impact of the latter, they help to alleviate symptoms of depression.
Monoamine Oxidise Inhibitors (MAOIs):
MAOIs work by reducing the activity of substances called monoamine oxidase enzymes, which break down neurochemicals such as serotonin, resulting in decreased levels at the synapse. By reducing the active breakdown, MAOIs help ensure a greater level of available serotonin for receptive neurons, associated with lessened depression.
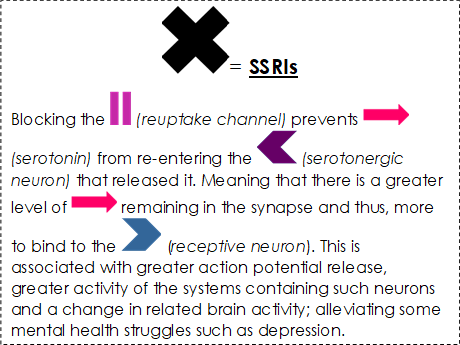
Serotonin Reuptake Inhibitors (SRIs):
As previously outlined, serotonin is one of the crucial neurochemicals in-relation to depression and other mental health struggles. Low levels of this neurotransmitter are associated with mental health problems. SRIs work by preventing serotonin from being taken back into serotonergic neurons post-release, meaning there are greater levels available at the synapse for utilisation by receptive neurons.
>>>>> SELECTIVE SEROTONIN REUPTAKE INHIBITORS >>>>>
(SSRIs)
(Now most commonly prescribed due to their lesser side effects.)
Whilst SSRIs work in the same fashion as SRIs, they are selective regarding which systems they impact and thus which processes/ feelings/ behaviours they influence. This impact is associated with neurochemical rebalancing within systems associated with depressive symptoms, and thus a reduction in mental health struggles.
SSRI Impact Upon Neurons:
Having some understanding of how such medications impact our internal workings can provide some reassurance and deeper understanding of ourselves. This is a reduced and simplified version of events and processes however, as we humans are beautifully complex. It is worth noting that it has been emphasised by recent studies that the changing of neurotransmitter levels (e.g. increasing serotonin), is likely only part of a more complicated process in-regards to altering mood and mental state. As there is on average a three-week delay between taking the first SSRI pill and subjectively noticing a change in one’s mental state, despite almost instantaneous changes in neurotransmitter levels. Nonetheless, understanding the relevance and function of neurochemicals gives us an insight into the biological explanation of mental struggles and sheds light on why so many of us are prescribed medications.
Part of a Bigger Picture:
Whilst the biomedical approach has contributed to great advancements in treating mental ill-health, it does not provide all the answers. This is emphasised by findings that suggest medications such as SSRIs have no significant impact on 10-30% of patients (Al-Harbi, 2012); one size does not fit all. Furthermore, research has found that placebo medication can be just as effective as antidepressants in some cases. Thus, there is more to the process of mental recovery than biological reactions of the drugs themselves.
To obtain a more holistic understanding, mental struggles and treatment paths should be approached from a biopsychosocial perspective (Toates, 2010). Bio standing for the biological approach previously outlined; psycho standing for psychological perspective relating to our cognition, internal mental frameworks, and thought patterns; and social relating to the social perspective of our relationships to others and wider networks. The biopsychosocial perspective emphasises how all these elements play a role in our mental state, equally important to one another and interactive at various levels. A change in one is reflected by a change in the other.
If we utilise a biological treatment of depression it can alleviate some depressive symptoms by changing neurotransmitter levels; in-turn this can lead to more positive thought patterns as our mood lifts; impacting our willingness to socialise and interact with others. Each interactive component contributes to alleviating depression.
The different components interact in a cyclical manner, but our mental state is a sum of the whole not just the individual factors. Whilst some of us may have experienced an eagerness from our medical professionals to prescribe ADMs, it is important that every element of the biopsychosocial framework is addressed in treating mental struggles.
Interventions From All Angles:
Biological
Medications > see your GP for further details and support.
Exercise > endorphins are released, a known feel good neurochemical.
Diet > eating healthy to support mental health.
Psychological
Therapies & interventions > one of the most utilised being cognitive-behavioural therapy.
Practising mindfulness > a therapeutic approach, but also a way of being in-touch with one’s self through activities such as meditation and journaling.
Thought mapping & tracking > fail to prepare, prepare to fail: schedule, structure and review your approach life.
Social
Be your own best friend > tune yourself to enjoy your own company, your favourite book or woodland walk.
Spend quality time > not everyone has to be your friend but make enjoyable memories with those who are.
Dogs are a man’s best friend > four-legged companions can be anyone’s best friend, therapy animals are used for a reason.
Understanding biological approaches and the medications that follow can help us to understand part of the journey we face on the way to treating mental health struggles such as depression. But it is important to acknowledge that they provide only one path on a map of many when pursuing mental health.
References
Al-Harbi, S, K. (2012): Treatment-resistant depression: therapeutic trends, challenges, and future directions, Patience preference and adherence, Dove Medical Press, 6, doi: 10.2147/PPA.S29716., pp. 369-388, Available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3363299/ , (Accessed 10/01/2020).
MIND (2013), Mental health facts and statistics. [Online]. Available at https://www.mind.org.uk/information-support/types-of-mental-health-problems/statistics-and-facts-about-mental-health/how-common-are-mental-health-problems/, (Accessed 15/01/2020).
Toates, F. (2010) Book 1: Core Concepts in Mental Health, SDK228 Module Team (eds), ‘Chapter 1: Explanations in mental health’, Milton Keynes, The Open University, pp. 1-27